Search
- Page Path
- HOME > Search
Invited Paper
- Lessons from the US Advanced Practice Registered Nurse system
- Eun-Ok Im, Dongmi Kim
- J Korean Acad Nurs 2025;55(4):492-505. Published online November 27, 2025
- DOI: https://doi.org/10.4040/jkan.25120
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This review compares the development of South Korea’s Advanced Practice Registered Nurse (APRN) system the well-established APRN system in the United States and provides recommendations for future improvements to the APRN system in South Korea.
Methods
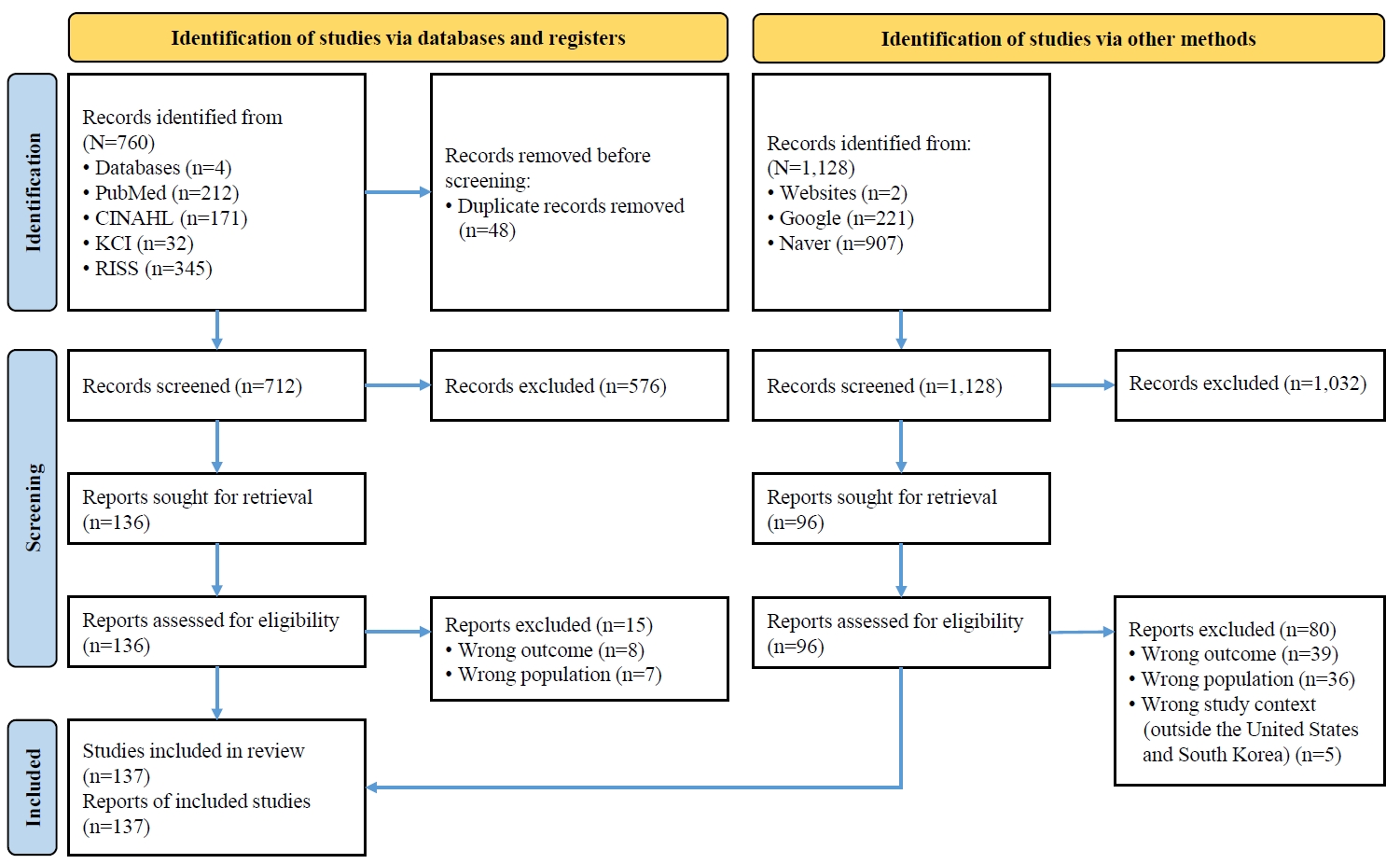
To compare the APRN systems between the two countries, an integrative literature review was conducted using multiple databases and professional nursing organization documents and reports from both the United States and South Korea.
Results
Issues were identified in five major domains: (1) research evidence, (2) education and training, (3) the scope of practice, (4) financial mechanisms, and (5) public awareness and acceptance.
Conclusion
Recommendations are made in four areas: (1) building evidence to support APRN programs; (2) strengthening APRN education; (3) establishing legal support and reimbursement mechanisms; and (4) improving public awareness and acceptance of APRNs.
- 780 View
- 118 Download

Research Paper
- Strategies for expanding the role of advanced practice providers in the Korean nursing workforce: a mixed-methods approach
- Jeong Hye Kim, Mi-Kyeong Jeon, Suyoung Choi, Mimi Lee, Su Jung Choi
- J Korean Acad Nurs 2025;55(4):568-583. Published online November 21, 2025
- DOI: https://doi.org/10.4040/jkan.25106

-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to propose strategies for strengthening the nursing workforce by expanding their roles as advanced practice providers (APPs).
Methods
A mixed-methods approach was employed, consisting of five focus group interviews (FGIs) with 30 healthcare professionals (including 10 physicians) and a two-round Delphi survey with 49 experts. The FGIs explored practical insights from clinical settings, while the Delphi process validated and prioritized strategic recommendations through expert consensus.
Results
Four major themes emerged from the FGI analysis: (1) utilization of diverse APPs to ensure quality care, (2) expanding the scope of practice of APPs, (3) requirements to ensure the quality of APPs, and (4) strategies for sustainable management of the APP workforce. Building on these findings, the Delphi survey identified five strategic domains: “definition and qualifications,” “scope of practice,” “educational programs,” “credentialing and regulation,” and “support systems.” Key areas of consensus included the need for mandatory clinical experience and specialty training, legal clarification of role boundaries, standardized curricula with certification mechanisms, and institution-led support systems such as task-specific job descriptions and recredentialing processes.
Conclusion
To effectively strengthen APP roles, it is essential to build on the existing advanced practice nurse (APN) framework, which already includes structured curricula and national certification. Furthermore, integrative strategies should be developed to incorporate experienced clinical nurses without APN licenses into the APN system.
- 1,449 View
- 126 Download

Review Paper
- Legal and Practical Solutions for the Expanding the Roles of Medical Support Staff Nurses
- Su Jung Choi, Min Young Kim
- J Korean Acad Nurs 2024;54(3):300-310. Published online August 31, 2024
- DOI: https://doi.org/10.4040/jkan.24075
-
 Abstract
Abstract
 PDF
PDF - Purpose
Medical support staff nurses have traditionally performed various supportive tasks for physicians, often extending beyond standard nursing roles. Despite these long-standing practices, there is a notable lack of official recognition and legal protection for these expanded responsibilities, leading to increasing legal concerns. Therefore, there is a need for proposing a rational solution to address these issues.
Methods
The number of medical support staff nurses is rising, particularly as they fill gaps left by the 2024 resident physician strike. The study focuses on identifying potential challenges arising from this shift and developing strategic improvements to address these challenges effectively.
Results
This study proposed legally expanding the scope of nursing duties and creating a robust system for training and certifying nurses to handle these responsibilities effectively, by integrating these roles within the advanced practice nurse (APN) framework.
Conclusion
Integrating these roles within the framework of APN can offer a sustainable and legally sound solution to the ongoing healthcare crisis, ensuring patient safety and safeguarding healthcare workers’ legal rights. -
Citations
Citations to this article as recorded by- Legislation of Medical Support Tasks in the Nursing Act as a Foundation for Nursing Professionalism and Role Expansion
Su Jung Choi
Korean Journal of Adult Nursing.2025; 37(2): 69. CrossRef - Role Transformation and Adaptation of Physician Assistants during the 2024 Medical Workforce Shortage: A Phenomenological Study
Tae Yeong Yang, Nahyun Lee
Journal of Korean Academy of Nursing Administration.2025; 31(3): 259. CrossRef - Effects of Role Conflict, Work Environment, and Meaning of Work on Job Embeddedness among Physician Assistants
Kwang Hoon Seo, Tae Yeong Yang, Nam Gyu Park, Jung Eun Park
Journal of Korean Academy of Nursing Administration.2025; 31(3): 249. CrossRef - Media discourse on physician assistant nurses in South Korea: a text network and topic modeling approach
Young Gyu Kwon, Daun Jeong, Song Hee Park, Mi Kyung Kim, Chan Woong Kim
Journal of Korean Academy of Nursing.2025; 55(3): 388. CrossRef - Comparison of educational needs and priorities for work-related laws between hospital and community-based nurses
Jeonghyun Kim, Min Kyoung Han, Minjae Lee, Sujin Shin
Journal of Korean Academy of Nursing.2025; 55(3): 400. CrossRef - Predictors of end-of-life care among emergency nurses: A cross-sectional study in Korea
Ji Seon Lee, Sook Jung Kang
Australasian Emergency Care.2025;[Epub] CrossRef - The Influence of Clinical Practice Nurses' Self-Leadership, Role Conflict, and Practice Environment on Patient Safety Competency
Jeong Hwa Heo, Ji Hyun Sung
Journal of Korean Academy of Nursing Administration.2025; 31(4): 458. CrossRef - Strategies for expanding the role of advanced practice providers in the Korean nursing workforce: a mixed-methods approach
Jeong Hye Kim, Mi-Kyeong Jeon, Suyoung Choi, Mimi Lee, Su Jung Choi
Journal of Korean Academy of Nursing.2025; 55(4): 568. CrossRef - Development and Psychometric Properties of the Korean Version of the Novice Nursing Practitioner Role Transition Scale
Eun Sook Kim, Mi-Kyeong Jeon, Su Jung Choi, Onam Ok, Genehee Lee, Ahyeong Song
Asian Nursing Research.2025; 19(5): 462. CrossRef
- Legislation of Medical Support Tasks in the Nursing Act as a Foundation for Nursing Professionalism and Role Expansion
- 5,122 View
- 293 Download
- 4 Web of Science
- 9 Crossref

Research Paper
- Intention to Delegate Clinical Practice of Medical Specialists in Accordance with the Enactment of the Scope of Practice for Advanced Practice Nurses
- Min Young Kim, Su Jung Choi, Jeong Hye Kim, Cho Sun Leem, Young-ah Kang
- J Korean Acad Nurs 2023;53(1):39-54. Published online February 28, 2023
- DOI: https://doi.org/10.4040/jkan.22098
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to investigate the nationwide intention to delegate clinical practice of medical specialists in accordance with the enactment of the scope of practice for advanced practice nurses (APNs).
Methods
Data were collected from October to December 2021 using Google Surveys. In total, 147 medical specialists from 12 provinces responded to the survey. The survey questionnaire was categorized into four legislative draft duties, according to the scope of practice (a total of 41 tasks): Twenty-nine tasks on treatments, injects, etc., performed under the guidance of a physician and other activities necessary for medical treatment (treatment domain); two tasks on collaboration and coordination; six tasks on education, counseling, and quality improvement; four regarding other necessary tasks. Participants were asked whether they were willing to delegate the tasks to APN.
Results
The intention to delegate tasks to APN was higher for non-invasive tasks such as blood sampling (97.3%) or simple dressing (96.6%). Invasive tasks such as endotracheal tube insertion (10.2%), sampling: bone marrow biopsy & aspiration (23.8%) showed low intention to delegate in the treatment domain. Participants who were older, male, and had more work careers with APN, showed a higher intention to delegate tasks.
Conclusion
To prevent confusion in the clinical setting, a clear agreement on the scope of APN practice as APN delegated by physicians should be established. Based on this study, legal practices that APN can perform legally should be established. -
Citations
Citations to this article as recorded by- Strategies for expanding the role of advanced practice providers in the Korean nursing workforce: a mixed-methods approach
Jeong Hye Kim, Mi-Kyeong Jeon, Suyoung Choi, Mimi Lee, Su Jung Choi
Journal of Korean Academy of Nursing.2025; 55(4): 568. CrossRef - Results of Applying a Ventilator Weaning Protocol Led by an Advanced Practice Nurse for Cardiac Surgery Patients
YoungJu Eim, Su Jung Choi
Journal of Korean Critical Care Nursing.2024; 17(2): 42. CrossRef - Legal and Practical Solutions for the Expanding the Roles of Medical Support Staff Nurses
Su Jung Choi, Min Young Kim
Journal of Korean Academy of Nursing.2024; 54(3): 300. CrossRef
- Strategies for expanding the role of advanced practice providers in the Korean nursing workforce: a mixed-methods approach
- 2,130 View
- 82 Download
- 3 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev