Search
- Page Path
- HOME > Search
Review Paper
- Risk factors for the readmission of patients with diabetic ketoacidosis: a systematic review and meta-analysis
- Hyerim Ji, Sun-Kyung Hwang
- J Korean Acad Nurs 2025;55(4):634-650. Published online November 21, 2025
- DOI: https://doi.org/10.4040/jkan.25072
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to identify risk factors associated with the readmission of patients with diabetic ketoacidosis (DKA) through a systematic review and meta-analysis.
Methods
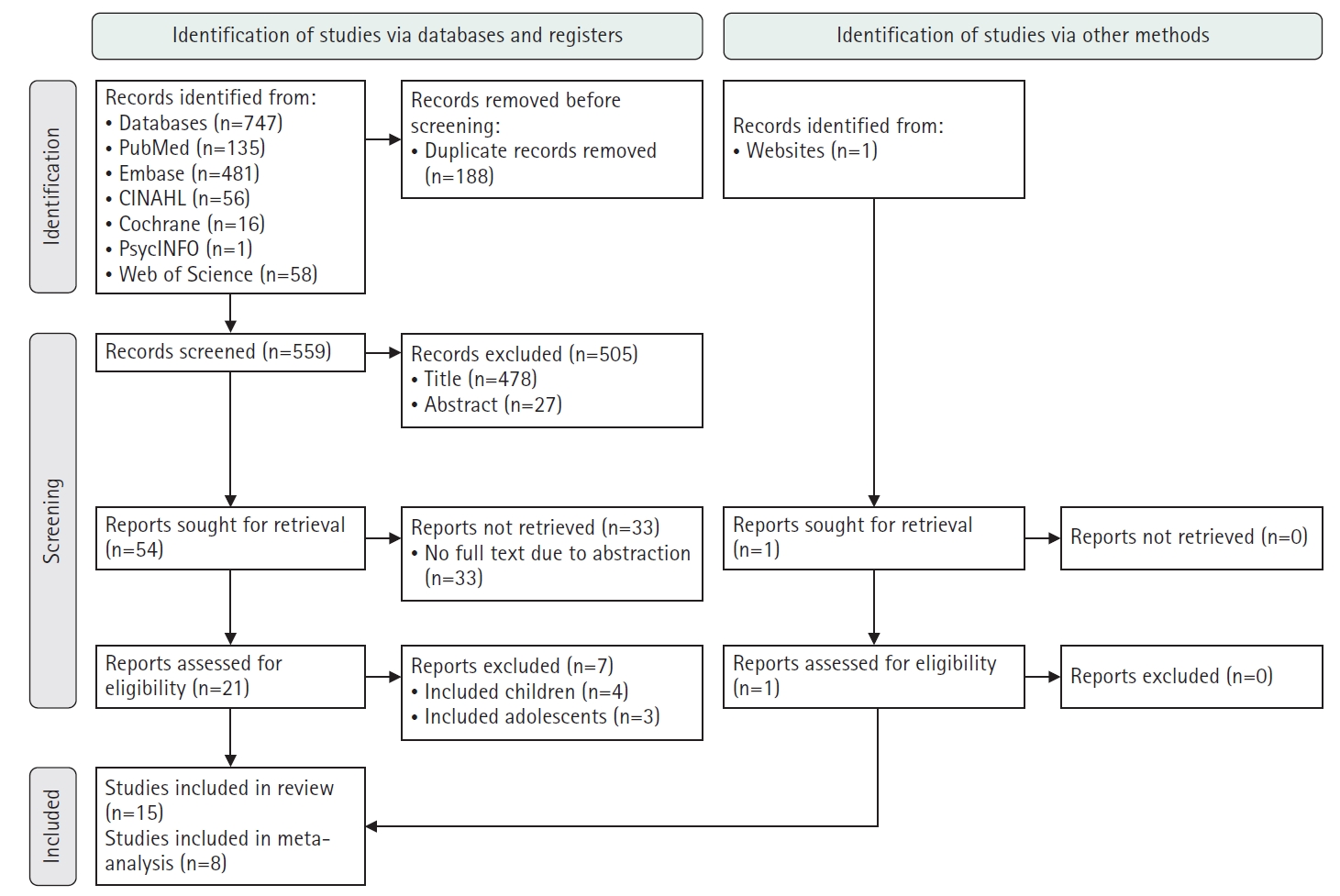
A systematic literature review was conducted in accordance with the PRISMA guidelines. Relevant studies were retrieved from international databases (PubMed, EMBASE, Cochrane Library, CINAHL, PsycINFO, and Web of Science) and Korean databases (RISS, KoreaMed, KMbase, KISS, and DBpia). Study quality was evaluated using the Newcastle-Ottawa Scale. Meta-analysis was performed using a random-effects model with the Hartung-Knapp-Sidik-Jonkman adjustment to account for the limited number of studies and heterogeneity.
Results
Fifteen studies were included in the review, and eight were eligible for meta-analysis. From the systematic review, 21 risk factors for DKA readmission were identified and categorized into five domains: demographic, socioeconomic, diabetes-related, comorbidity, and health-behavioral factors. In the meta-analysis, significant risk factors included low income, psychiatric disorders, and discharge against medical advice.
Conclusion
This study demonstrates that DKA readmissions result from the complex interplay of multiple clinical and social factors. By identifying these risk factors and suggesting risk-stratification criteria, the findings may support the development of tailored interventions, such as self-management education, integrated mental health care, structured discharge planning, and coordinated post-discharge follow-up.
- 1,058 View
- 151 Download

Research Papers
- Development of a machine learning-based prediction model for early hospital readmission after kidney transplantation: a retrospective study
- Hye Jin Chong, Ji-hyun Yeom
- J Korean Acad Nurs 2025;55(4):528-542. Published online November 21, 2025
- DOI: https://doi.org/10.4040/jkan.25030
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to develop and validate a machine learning-based prediction model for early hospital readmission (EHR) post-kidney transplantation.
Methods
The study was conducted at the organ transplantation center of a university hospital, utilizing data from 470 kidney transplant recipients. We built and trained four machine learning models and tested them to identify the strongest EHR predictors. Predictive performance was evaluated using confusion matrices and the area under the receiver operating characteristic curve (ROC AUC).
Results
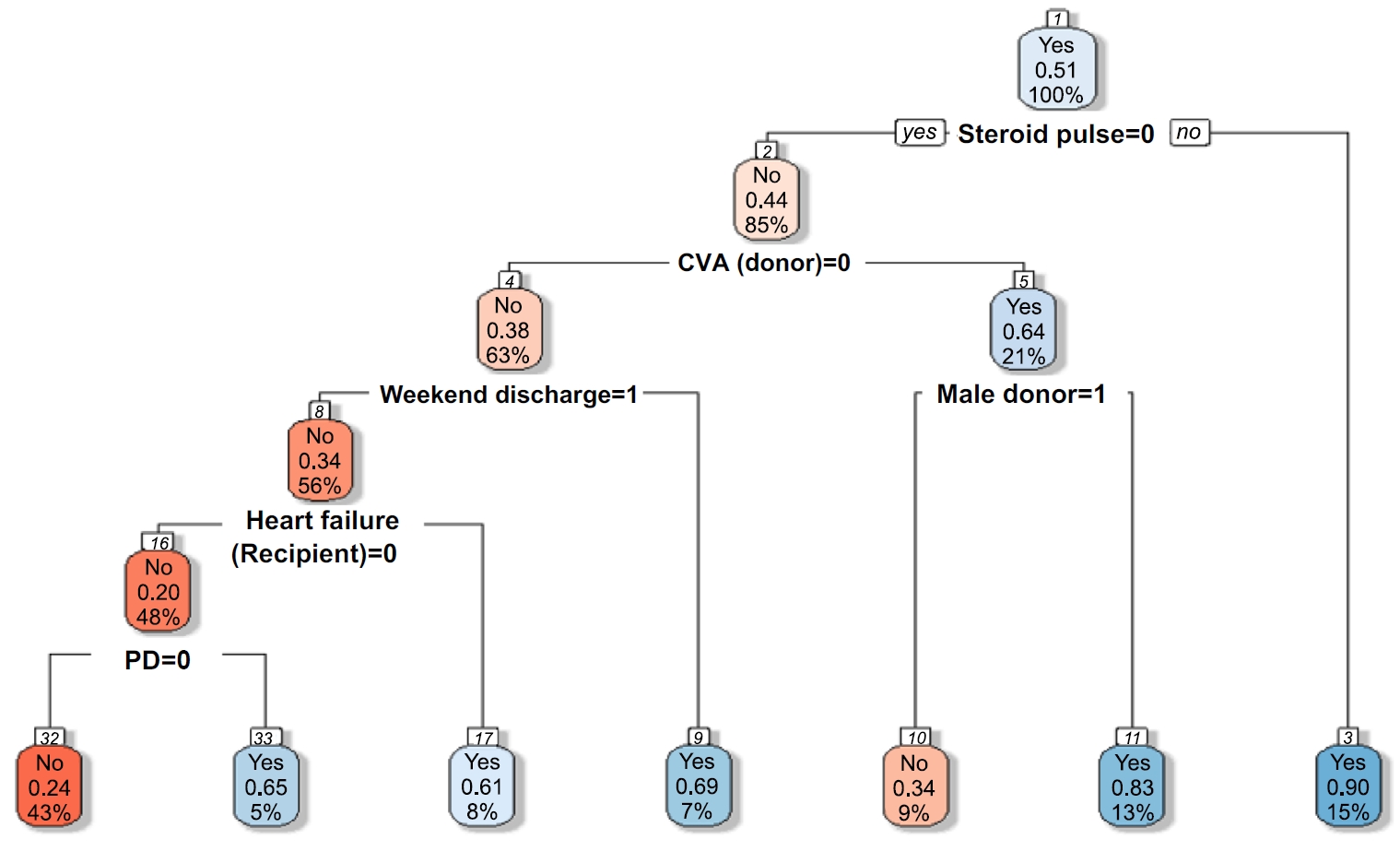
Among the 470 kidney transplant recipients with a mean age of 46.1 ± 12.02 years, 322 (68.5%) were males, and 74 (15.7%) were readmitted within 30 days after kidney transplantation. In total, 241 (51.2%) recipients were found to have experienced EHR after applying the random over-sampling examples method. The random forest model achieved the best performance, with an ROC AUC of .87 (validation set) and .82 (test set). The 15 most important features were steroid pulse therapy (recipient), cerebrovascular accident (recipient), heart failure (recipient), male sex (donor), cardiovascular disease (recipient), weekend discharge (recipient), peritoneal dialysis (recipient) cerebrovascular accident as the cause of brain death (donor), current smoker (recipient), cardiac arrest (donor), previous kidney transplantation (recipient), age (donor), hypertension (donor), male sex (recipient), and dialysis duration (recipient).
Conclusion
Our framework demonstrated strong predictive interpretability. It can support appropriate and effective clinical decision-making by assisting transplant professionals in stratifying recipients based on their risk of EHR. prioritizing post-discharge care and follow-up for high-risk individuals, and allocating targeted interventions such as closer monitoring or education.
- 974 View
- 125 Download

- Cut-Off Values of the Post-Intensive Care Syndrome Questionnaire for the Screening of Unplanned Hospital Readmission within One Year
- Jiyeon Kang, Yeon Jin Jeong, Jiwon Hong
- J Korean Acad Nurs 2020;50(6):787-798. Published online December 31, 2020
- DOI: https://doi.org/10.4040/jkan.20233
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to assign weights for subscales and items of the Post-Intensive Care Syndrome questionnaire and suggest optimal cut-off values for screening unplanned hospital readmissions of critical care survivors.
Methods
Seventeen experts participated in an analytic hierarchy process for weight assignment. Participants for cut-off analysis were 240 survivors who had been admitted to intensive care units for more than 48 hours in three cities in Korea. We assessed participants using the 18-item Post-Intensive Care Syndrome questionnaire, generated receiver operating characteristic curves, and analysed cut-off values for unplanned readmission based on sensitivity, specificity, and positive likelihood ratios.
Results
Cognitive, physical, and mental subscale weights were 1.13, 0.95, and 0.92, respectively. Incidence of unplanned readmission was 25.4%. Optimal cut-off values were 23.00 for raw scores and 23.73 for weighted scores (total score 54.00), with an area of under the curve (AUC) of .933 and .929, respectively. There was no significant difference in accuracy for original and weighted scores.
Conclusion
The optimal cut-off value accuracy is excellent for screening of unplanned readmissions. We recommend that nurses use the Post-Intensive Care Syndrome Questionnaire to screen for readmission risk or evaluating relevant interventions for critical care survivors. -
Citations
Citations to this article as recorded by- Cutoff Values for Screening Post-Intensive Care Syndrome Using the Post-Intensive Care Syndrome Questionnaire
Jiwon Hong, Jiyeon Kang
Journal of Clinical Medicine.2025; 14(11): 3897. CrossRef - Translation and validation of the Chinese version of the post-intensive care syndrome questionnaire
Caidie Yang, Hongmei Wu, Chunmei Luo
BMC Nursing.2025;[Epub] CrossRef - Post‐Intensive Care Syndrome in Family: A Concept Analysis
Jiaqi Wen, Zhenjing Hu, Ziwei Li, Yu Liu, Liting Zhang, Chenchen Zhong
Scandinavian Journal of Caring Sciences.2025;[Epub] CrossRef - Post intensive care syndrome: A review of clinical symptoms, evaluation, intervention
Xiaofang He, Yuwei Song, Yuchun Cao, Liying Miao, Bin Zhu
Heliyon.2024; 10(10): e31278. CrossRef - Screening tools for post–intensive care syndrome and post-traumatic symptoms in intensive care unit survivors: A scoping review
Usha Pant, Krooti Vyas, Shaista Meghani, Tanya Park, Colleen M. Norris, Elizabeth Papathanassoglou
Australian Critical Care.2023; 36(5): 863. CrossRef
- Cutoff Values for Screening Post-Intensive Care Syndrome Using the Post-Intensive Care Syndrome Questionnaire
- 2,657 View
- 64 Download
- 5 Web of Science
- 5 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev