Search
- Page Path
- HOME > Search
Research Paper
- Job stress levels and coping among hospital nurses: a latent profile analysis
- Myungji Kim, Hyunkyung Choi
- J Korean Acad Nurs 2025;55(3):377-387. Published online August 22, 2025
- DOI: https://doi.org/10.4040/jkan.25061
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to identify job stress levels and coping profiles among hospital nurses, explore the factors influencing profile classification, and determine whether levels of job embeddedness and happiness varied among the profiles.
Methods
Data were collected through an online survey of 325 hospital nurses, and latent profiles were identified via latent profile analysis. The R3STEP (three-step auxiliary variable approach) method was used to examine the factors influencing the latent profiles, and one-way analysis of variance was conducted to analyze differences in levels of job embeddedness and happiness.
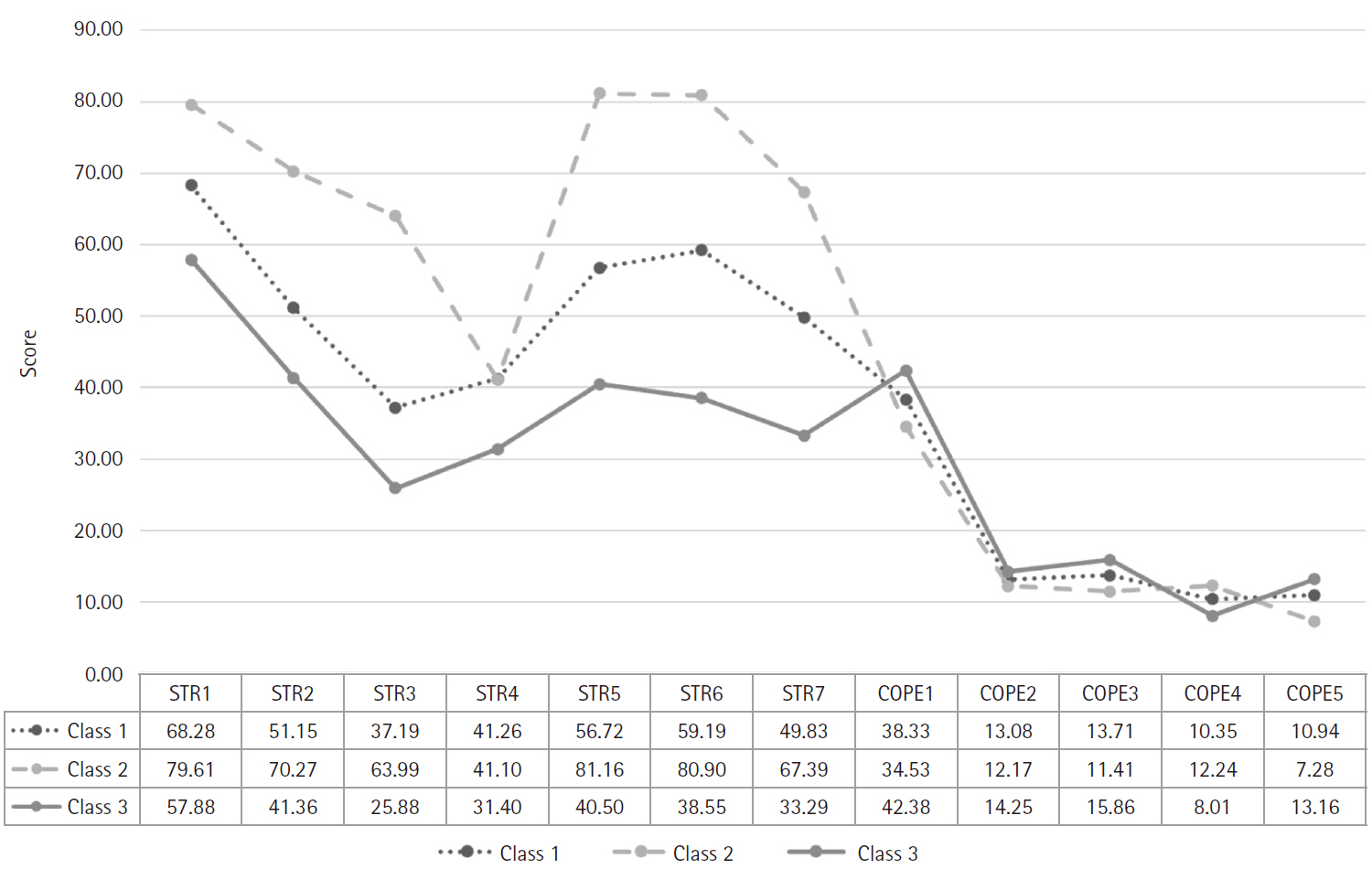
Results
Three job stress and coping profiles were identified: (1) the “moderate stress-balanced coping group”, characterized by moderate levels of job stress and moderate use of all coping strategies; (2) the “high stress-emotional coping group”, with high job stress and primary use of emotional display strategies; and (3) the “low stress-adaptive coping group, with low job stress and the utilization of a variety of coping strategies. Workplace location and monthly income influenced the classification of latent profiles. Nurses working in metropolitan areas and those with lower monthly incomes were more likely to be classified into the high stress-emotional coping group than other groups. The levels of job embeddedness and happiness were highest in the low stress-adaptive coping group and lowest in the high stress-emotional coping group.
Conclusion
The results of this study indicate the need to develop strategies that offer diverse stress-coping programs and support nurses in effectively utilizing coping methods that best suit their individual needs.
- 2,050 View
- 227 Download

Original Article
- Predictors of Blood and Body Fluid Exposure and Mediating Effects of Infection Prevention Behavior in Shift-Working Nurses: Application of Analysis Method for Zero-Inflated Count Data
- Jae Geum Ryu, Choi-Kwon Smi
- J Korean Acad Nurs 2020;50(5):658-670. Published online October 31, 2020
- DOI: https://doi.org/10.4040/jkan.20025
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to identify the predictors of blood and body fluid exposure (BBFE) in multifaceted individual (sleep disturbance and fatigue), occupational (occupational stress), and organizational (hospital safety climate) factors, as well as infection prevention behavior. We also aimed to test the mediating effect of infection prevention behavior in relation to multifaceted factors and the frequency of BBFE.
Methods
This study was based on a secondary data analysis, using data of 246 nurses from the Shift Work Nurses’ Health and Turnover study. Based on the characteristics of zero-inflated and over-dispersed count data of frequencies of BBFE, the data were analyzed to calculate zero-inflated negative binomial regression within a generalized linear model and to test the mediating effect using SPSS 25.0, Stata 14.1, and PROCESS macro.
Results
We found that the frequency of BBFE increased in subjects with disturbed sleep (IRR = 1.87, p = .049), and the probability of non-BBFE increased in subjects showing higher infection prevention behavior (IRR = 15.05, p = .006) and a hospital safety climate (IRR = 28.46, p = .018). We also found that infection prevention behavior had mediating effects on the occupational stress-BBFE and hospital safety climate-BBFE relationships.
Conclusion
Sleep disturbance is an important risk factor related to frequency of BBFE, whereas preventive factors are infection prevention behavior and hospital safety climate. We suggest individual and systemic efforts to improve sleep, occupational stress, and hospital safety climate to prevent BBFE occurrence. -
Citations
Citations to this article as recorded by- Development of an infection control competency scale for clinical nurses: an instrument design study
Yong Hwan Hyeon, Kyoung Ja Moon
BMC Nursing.2024;[Epub] CrossRef - Work Characteristics and Needlestick-Injury Status of Dental Hygienists
Yeon-Soon Park, Jeong-Hyun Lee, Jin-Soo Kim, Kyoung-Ok Yun, Sung-Suk Bae
Journal of Dental Hygiene Science.2024; 24(3): 190. CrossRef - Smartphone‐based home workout program for shift‐work nurses working during the COVID‐19 pandemic
Yunmi Baek, Kihye Han, Jieun Kim, Hae Young Yoo
Nursing & Health Sciences.2022; 24(3): 708. CrossRef - Mediating Effects of Role Clarity between Clinical Decision-Making Abilities and Job Stress for Advanced Practice Nurses at Tertiary Hospitals
Min Young Kim, Jeong Hye Kim, Su Jung Choi
Journal of Korean Critical Care Nursing.2022; 15(2): 27. CrossRef
- Development of an infection control competency scale for clinical nurses: an instrument design study
- 1,556 View
- 40 Download
- 2 Web of Science
- 4 Crossref

Research Paper
- Secondary Data Analysis on the Factors Influencing Premenstrual Symptoms of Shift Work Nurses: Focused on the Sleep and Occupational Stress
- Jihyun Baek, Smi Choi-Kwon
- J Korean Acad Nurs 2020;50(4):631-640. Published online August 31, 2020
- DOI: https://doi.org/10.4040/jkan.19230
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to examine premenstrual symptoms (PMS) of shift nurses and identify the association between PMS, sleep, and occupational stress.
Methods
This study was conducted with a secondary data analysis that used data from the Shift Work Nurse’s Health and Turnover study. The participants were 258 nurses who were working in shifts including night shifts. PMS, sleep patterns (sleep time and sleep time variability), sleep quality, and the occupational stress of each participant were measured using the Moos Menstrual Distress Questionnaire, a sleep diary, an actigraph, the Insomnia Severity Index, and the Korean Occupational Stress Scale, respectively. Data were analyzed using SPSS 23 and STATA 15.1 to obtain descriptive statistics, Pearson’s correlation coefficients, multiple linear regression with generalized estimating equations (GEE) and Baron and Kenny’s mediating analysis.
Results
The average PMS score, average sleep time, average sleep time variability, average sleep quality score, and average occupational stress score of the participants was 53.95 ± 40.45, 7.52 ± 0.89 hours, 32.84 ± 8.43%, 12.34 ± 5.95, and 49.89 ± 8.98, respectively. A multiple linear regression analysis with GEE indicated that sleep time variability (B = 0.86, p = .001), and sleep quality (B = 2.36, p < .001) had negative effects on nurses’ PMS. We also found that sleep quality had a complete mediating effect in the relationship between occupational stress and PMS.
Conclusion
These findings indicate that both sleep time variability and sleep quality are important factors associated with PMS among shift work nurses. To improve shift nurses’ PMS status, strategies are urgently needed to decrease sleep time variability and increase sleep quality. -
Citations
Citations to this article as recorded by- Hospital Nurses’ Professional Quality of Life Model: A Cross‐Sectional Study Based on the Expanded Job Demands‐Resources Model
Younghee Kim, Mi Yu, Jacopo Fiorini
Journal of Nursing Management.2025;[Epub] CrossRef - Premenstrual Symptoms Risk Factors Among Newly Graduated Nurses in Shift Work: A Prospective Longitudinal Study
Iksoo Huh, Smi Choi-Kwon, Jison Ki, Soyeon Kim, Jihyun Baek
Asian Nursing Research.2024; 18(5): 501. CrossRef - Premenstrual Syndrome’s Impact on Work-Related Quality of Life Among Jordanian Nurses
Yamamah Al-Hmaid, Othman Beni Yonis, Mais Alkhalili, Khalid Kheirallah
Cureus.2024;[Epub] CrossRef - Investigating influencing factors on premenstrual syndrome (PMS) among female college students
Su Jeong Yi, Miok Kim, Ina Park
BMC Women's Health.2023;[Epub] CrossRef - Development and validation of risk prediction model for premenstrual syndrome in nurses: results from the nurses-based the TARGET cohort study
Li Li, Xiaoyan Lv, Yuxin Li, Xinyue Zhang, Mengli Li, Yingjuan Cao
Frontiers in Public Health.2023;[Epub] CrossRef - Shift nurses’ social jetlag, anxiety, and premenstrual symptoms: A cross-sectional study
Taeyeon Kim, Sun Joo Jang
Collegian.2022; 29(4): 477. CrossRef - Depressive symptoms and menstrual distress according to the menstrual phase in nurses: the Korea Nurses’ Health Study
Oksoo Kim, Sue Kim, Hae Ok Jeon, Ahrin Kim, Chiyoung Cha, Bohye Kim
Journal of Psychosomatic Obstetrics & Gynecology.2022; 43(4): 541. CrossRef - Secondary Data Analysis on the Quality of Sleep and Related Factors of Novice and Experienced Shift Work Nurses
Minjeong Yu, Smi Choi-Kwon
Journal of Korean Academy of Nursing.2020; 50(5): 646. CrossRef
- Hospital Nurses’ Professional Quality of Life Model: A Cross‐Sectional Study Based on the Expanded Job Demands‐Resources Model
- 1,949 View
- 85 Download
- 10 Web of Science
- 8 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev